A surprising fix in aging joints
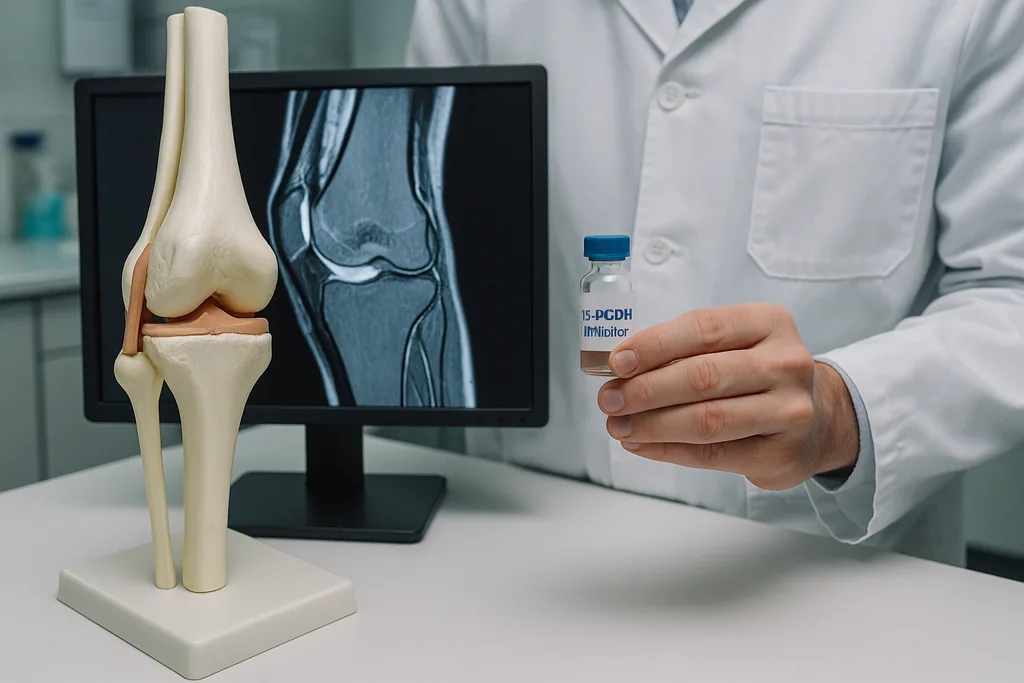
This week Stanford Medicine published results showing that a small‑molecule inhibitor of an age‑associated enzyme can reverse cartilage loss in old mice and reduce the chance of arthritis after knee injuries. The study, published online in Science on 27 November 2025 and summarised by Stanford and ScienceDaily in January 2026, reports that blocking 15‑hydroxy prostaglandin dehydrogenase (15‑PGDH) thickened articular cartilage in aged animals, restored a youthful gene expression profile in chondrocytes and triggered early signs of repair in human cartilage samples taken from knee‑replacement surgeries. The experiments used both systemic dosing and direct injections into the joint; in injury models that mimic ACL tears, treated animals were far less likely to develop osteoarthritis and recovered more normal weight‑bearing behaviour.
The biology: 15‑PGDH, prostaglandins and cell reprogramming
Instead of recruiting new stem or progenitor cells, the treated cartilage's resident chondrocytes changed their gene‑expression programs and shifted toward a more youthful state. Single‑cell analyses in the paper reported clear shifts in cell populations: a small group of chondrocytes that produced 15‑PGDH and cartilage‑degrading enzymes fell from about 8% of cells to 3% after treatment; cells associated with fibrocartilage (a less functional repair tissue) declined from ~16% to ~8%; and a population linked to healthy hyaline articular cartilage rose from ~22% to ~42%. Those numbers point to broad molecular reprogramming across the tissue rather than the arrival of new cartilage‑forming stem cells.
Evidence from mice, injury models and human tissue
The researchers tested the inhibitor in three complementary ways. First, in aged mice with naturally thinned knee cartilage the drug—given either systemically or injected into the joint—produced measurable thickening of the articular surface and restored features of hyaline cartilage rather than scar‑like fibrocartilage. Second, in surgical injury models that mimic anterior cruciate ligament (ACL) tears, mice that received twice‑weekly injections for four weeks after injury were significantly less likely to develop osteoarthritis than control animals; untreated animals developed OA within weeks and showed elevated 15‑PGDH. Behaviorally, treated mice placed more weight on their injured leg and moved more normally.
Third, and crucial for clinical relevance, human cartilage samples removed during total knee replacement were exposed to the inhibitor ex vivo. After one week the tissues showed fewer 15‑PGDH–expressing chondrocytes, reduced expression of genes tied to cartilage degradation and fibrocartilage, and early molecular signs of articular cartilage regeneration. That ex vivo response does not prove success in living patients, but it reduces one of the big translational uncertainties that often sink preclinical findings.
Routes to the clinic and prior safety data
The Stanford team emphasised two practical paths forward: a targeted intra‑articular injection and an oral small molecule. Notably, Phase 1 trials of a 15‑PGDH inhibitor conducted for age‑related muscle weakness have already shown the compound to be safe and biologically active in healthy volunteers, according to the authors. That existing human safety data is important because it can accelerate first‑in‑human trials specifically designed to test cartilage repair. The paper's senior authors said they hope a cartilage‑focused Phase 1 study will be launched soon.
Still, the difference between systemic and local dosing matters. Systemic dosing can shift prostaglandin signalling across organs, so trials will need to monitor effects beyond the joint. The investigators also describe intra‑articular injections into the knee as a feasible approach: local delivery concentrates the drug where it is needed and could reduce off‑target consequences elsewhere in the body. The published work used both strategies successfully in mice.
Conflicts, intellectual property and collaborators
Open questions and caveats
This is exciting preclinical evidence, but several major unknowns remain. The experiments were performed in mice and in human tissue kept alive in the lab; neither alone proves that injections or pills will regrow functional cartilage in living people or halt long‑term osteoarthritis progression. The mechanism—raising PGE2 by blocking its degradation—can have different effects in different tissues and contexts: PGE2 is implicated both in regenerative signalling and in inflammatory pain. Careful dose‑finding, safety monitoring and long‑term follow‑up will be essential in human trials to watch for unexpected inflammatory or proliferative consequences.
Regeneration of true, load‑bearing hyaline cartilage is notoriously difficult, and many promising strategies have failed or produced only modest clinical benefit. Nevertheless, the combination of strong effects in aged animals, protection after injury and an early positive signal in human explants makes this one of the more persuasive preclinical claims for a disease‑modifying osteoarthritis therapy in recent years.
What this could mean for patients and health systems
If the effect translates to people, the implications are substantial. Osteoarthritis affects roughly one in five adults in the United States and accounts for tens of billions of dollars in direct health‑care costs each year. A drug or targeted injection that regenerated cartilage or prevented post‑injury OA would change clinical practice: instead of only treating pain and, eventually, replacing joints surgically, physicians might be able to restore tissue function earlier and reduce the need for expensive joint replacements.
For patients facing years of pain or the prospect of joint surgery, the idea of regrowing one’s own cartilage from existing cells is transformational. But translating a laboratory breakthrough into a safe, scalable therapy takes time and rigorous clinical evidence. The next steps are clear: carefully designed human trials, independent replication, and close safety monitoring. For now the result is a powerful proof of concept and a prompt for accelerated clinical work.
Sources
- Science (research paper on 15‑PGDH inhibition and cartilage regeneration)
- Stanford Medicine press materials and news release
- Sanford Burnham Prebys Medical Discovery Institute (collaborating institution)
- National Institutes of Health (grant support listed in the study)
Comments
No comments yet. Be the first!